Lower Acute Healthcare Utilization Associated with Virtual Cardiometabolic Health Programs
Susan M. Devaraj PhD, MS, RD, LDN, Jenna Napoleone, PhD, MPH; Madison Noble, MPH; Christina M Parrinello, PD; Carolyn Jasik, MD; Sarah Linke PhD, MPH
Originally presented at AHA EPI | Lifestyle Scientific Sessions 2025
Abstract
Background
Type 2 diabetes and hypertension are common and costly conditions that increase risk for hospitalization. Lifestyle-focused virtual health programs may offer an effective and accessible self-management solution for these conditions and reduce future high-cost acute care encounters. The purpose of this study was to evaluate the differences in inpatient and emergency room (ER) healthcare utilization between patients enrolled in a virtual health program (VH) for cardiometabolic lifestyle management vs. usual care (UC) controls at 6 and 12 months.
Methods
We conducted a real-world, retrospective secondary analysis of healthcare claims incurred between July 2019 and May 2023 from multiple payers. Inclusion criteria included continuous coverage for ≥6 months pre- and post-index, an age range of 18-64 years, and having commercial insurance. Index date was defined as the program enrollment date for VH patients or an outpatient claim with a type 2 diabetes and/or hypertension diagnosis code for UC patients. VH patients were enrolled in Omada for Diabetes (DM; n=317), Hypertension (HTN; n=1,102), or DM+HTN (n=315) program and 1:3 propensity score matched (demographics, clinical characteristics and pre-index costs) to UC controls (n=951, n=3,306, and n=945, respectively). Mean differences in post-index inpatient, ER, and acute (inpatient+ER) encounter counts were compared at 6 and 12 months using t-tests.
Results
After matching, the VH and UC groups had no statistically significant differences in pre-index characteristics. VH patients across all programs had fewer inpatient, ER, and acute encounters at 6 and 12 months vs. UC (absolute mean difference range -0.01 to -0.33, relative difference range: -5% to -63%). Specifically, DM VH patients had 63% lower inpatient utilization at 12 months, 46% lower ER utilization at 6 months, and 54% and 52% lower acute utilization at both 6 and 12 months vs. UC (all p<.05). HTN VH patients experienced significant reductions at both 6 and 12 months for ER and acute utilization vs. UC (ER: -56%, -43%; Acute: -51%, -40%; all p<.05). Finally, DM+HTN patients had 43% lower ER utilization at 6 months vs. UC (p=.04).
Conclusion
Using a lifestyle-focused virtual health program to support cardiometabolic disease management may lead to meaningful reductions in high-cost acute care encounters, indicating the value of using virtual solutions as an effective and accessible approach to between-visit care.
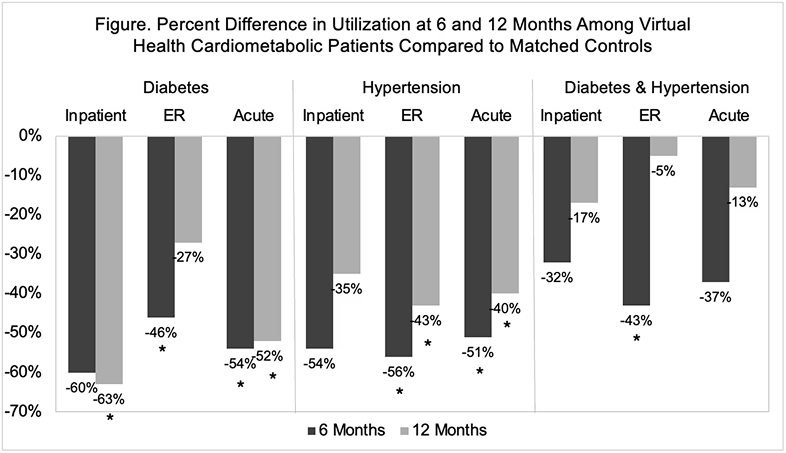
Relative differences in mean encounter counts were calculated as ([(VH - UC) / UC] * 100).
Findings presented at AHA EPI | Lifestyle Scientific Sessions 2025
