Know Your Numbers: How Diabetes Impacts Cholesterol and Cardiovascular Health
By Carolyn Salter, RD, LD, CDCES
This edition covers:
- The connection between diabetes and high cholesterol
- The challenges of managing multiple conditions
- Caring for individuals vs. individual conditions
For most people, November brings cooler weather, shorter days, and of course, Thanksgiving. However, November is also National Diabetes Awareness Month. As a Certified Diabetes Care and Education Specialist (CDCES), this month is my [insert big football game I’m not legally allowed to mention here.] Not because diabetes is fun, or a spectator sport, but because all eyes are on a chronic condition that affects millions of Americans every day. This month exists to raise awareness of the growing prevalence of diabetes, along with its burdens and complexities, and its impact on the rest of our bodily systems.
People with diabetes are two to four times more likely to develop cardiovascular disease, aka heart disease, which is the leading cause of death globally.
While these aren’t the most uplifting statistics, knowing that diabetes and heart disease are connected is an important first step to preventing further health risks and complications.
That’s why this Diabetes Awareness Month we’re focusing on the connection between diabetes and cholesterol; more specifically, what the lab numbers mean, and why these conditions should be cared for together, not separately.
But first, I would be remiss to write an article about diabetes and cholesterol without defining what they are. So, before we put the cart in front of the horse, let’s start there.
What is Diabetes?
Diabetes occurs when the body’s blood glucose levels are too high due to the body not making enough or any insulin, or when the body doesn’t respond to the effects of insulin as it should. Insulin is the hormone made by the pancreas that helps the body utilize blood glucose properly. There are two main types of diabetes, type 1 and type 2.
In type 1 diabetes, an autoimmune disease formerly referred to as juvenile diabetes (but now more adults are being diagnosed,) the body doesn’t make insulin at all. People with type 1 diabetes need to take insulin to survive.
Type 2 diabetes, the most common form, doesn’t always require taking insulin, but oftentimes medication is needed alongside lifestyle modifications to help the body regulate blood sugar levels.
The A1C test is a common lab test used to measure average blood glucose levels over the previous two to three months, and testing cadence is based on several factors, including how controlled somebody’s blood glucose levels are. It is used to diagnose and monitor diabetes.
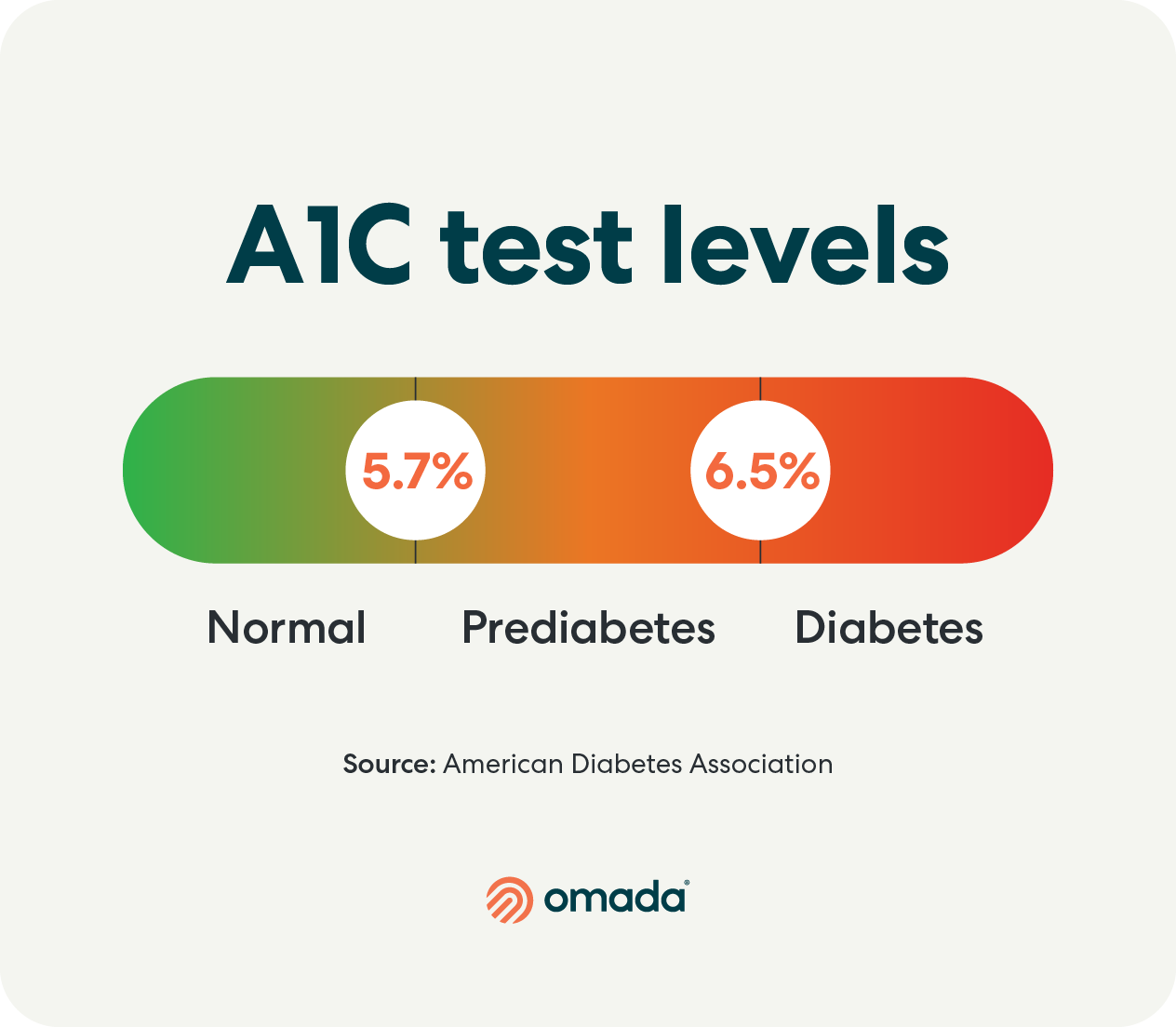
- An A1C level between 5.7 and less than 6.5 is in the pre-diabetes range.
- An A1C level of 6.5% or higher indicates diabetes range.
What is Cholesterol?
Cholesterol is a waxy, fatty substance made naturally by the body and is found in the blood. It’s also found in animal-based foods like dairy products and meat.
Cholesterol can be a great thing in small amounts. It can help protect nerves, generate cell tissue, and even plays an important role in hormone production. However, too much cholesterol can lead to health problems, especially in the presence of another condition like diabetes.
PThe American Heart Association (AHA) recommends that adults with diabetes have regular lipid panels to monitor their cholesterol levels.
What gets checked in a lipid panel and what the numbers mean:
Low-density lipoprotein (LDL) cholesterol: Also known as “bad” cholesterol, LDL sticks to the walls of the blood vessels, and can eventually block blood flow. The higher the amount of LDL, the higher the risk of heart problems or stroke.
- For adults with diabetes, the American Heart Association recommends an LDL level of <70 mg/dL.
- For adults without diabetes or heart disease, optimal LDL is at or below 100 mg/dL.
High-density lipoprotein (HDL) cholesterol: This “good” cholesterol collects extra LDL cholesterol in the body and takes it to the liver where it’s broken down. High levels of HDL are linked to a lower risk of heart disease.
- For adults, regardless of health status, current published recommendations are, >40 for men and >50 for women in protecting against heart disease.
Triglycerides: If the body consumes more calories than it needs, the excess is transformed into this type of fat in your blood. Excess calories from sugar and alcohol also turn into triglycerides. Like LDL cholesterol, triglycerides can build up inside the arteries and increase risk of serious issues.
- For people with diabetes, a triglyceride target of <150 mg/dL is recommended. The same triglyceride target is recommended for people without diabetes.
How Diabetes and Cholesterol are Connected
Next, let’s put it all together and talk about how diabetes can impact cholesterol levels.
Studies show a link between insulin resistance (which can lead to type 2 diabetes) and high cholesterol. Diabetes is also shown to lower “good” cholesterol and raise “bad” cholesterol levels, resulting in a condition called diabetic dyslipidemia. This condition can raise the risk of serious heart conditions, including coronary heart disease and atherosclerosis.
On the flip side, improving blood sugar levels can have a significantly positive effect on heart health. One study found that for every one-point reduction in A1C:
- The risk of heart attack declines by 14%
- The risk of stroke declines by 12%
- The risk of heart failure decreases by 16%
- The risk of all-cause mortality decreases by 14%
Multiple Conditions Can Lead to Complicated Care
Needless to say, managing diabetes and high cholesterol is a lot to manage for one person, especially within a complex healthcare system. Someone may encounter confusing results or a lack of support and guidance between doctor’s visits, all of which can contribute to diabetes distress. Social Drivers/Determinants of Health (SDOH) complicate things further, as they are environmental factors that impact health and quality of life, and can limit one’s access to healthy food and necessary healthcare.
Contradicting Dietary Guidelines
At the highest level, people with diabetes are commonly advised to pay close attention to their carbohydrate intake, while those with high cholesterol are recommended to reduce red fatty meats and full-fat dairy.
At the same time, the ketogenic diet (high fat, low carbohydrate) has risen in popularity as a recommendation for managing diabetes, given its effectiveness in improving blood sugar. Meanwhile, other studies suggest that the keto diet can significantly raise LDL (bad cholesterol). This contradicting information further exacerbates the complexities of managing diabetes and cholesterol through diet.
Confusing Lab Results
We’ve all been there. Our lab results come through on the patient portal, and we look at the numbers. Then we scour the internet to find out if we’re healthy or not. Then the search results give us several different answers, and we’ve gone down a rabbit hole of potential health misinformation before our doctor can even assess our results.
Lack of Lifestyle Support
It is estimated that people with type 1 diabetes can make about 120 additional decisions per day when it comes to their health. And so often, people managing chronic conditions are doing so on their own without clinical support in the weeks or months between doctor’s visits. From my experience in the field of diabetes care, this is where many people struggle. They will have a great week of healthy habits, experience a few missteps, feel overwhelmed by trying to do it all, and give up. And trust me, it wasn’t from lack of desire to change.
Life can get complicated, and for many Omada members I’ve worked with, the thought of changing their lifestyle to manage their cholesterol along with their diabetes leaves them feeling defeated. Many feel they take one step forward (made it to the gym after work!) then take two steps back (donuts in the break room.) The “well-meaning” family advice, trying to cook healthy while trying to keep a spouse and kids happy, the contradicting social media posts, commercials for unhealthy foods, checking glucose multiple times today, remembering to attend doctor visits, it’s all too much. So what options are there for people managing multiple conditions at once?
Effective Care Means Treating the Individual, not Individual Conditions
For people managing multiple conditions, such as diabetes and high cholesterol, caring for the individual person instead of simply treating individual conditions is paramount to their success.
Here’s what that looks like:
Building and Supporting Healthy Behavior Change
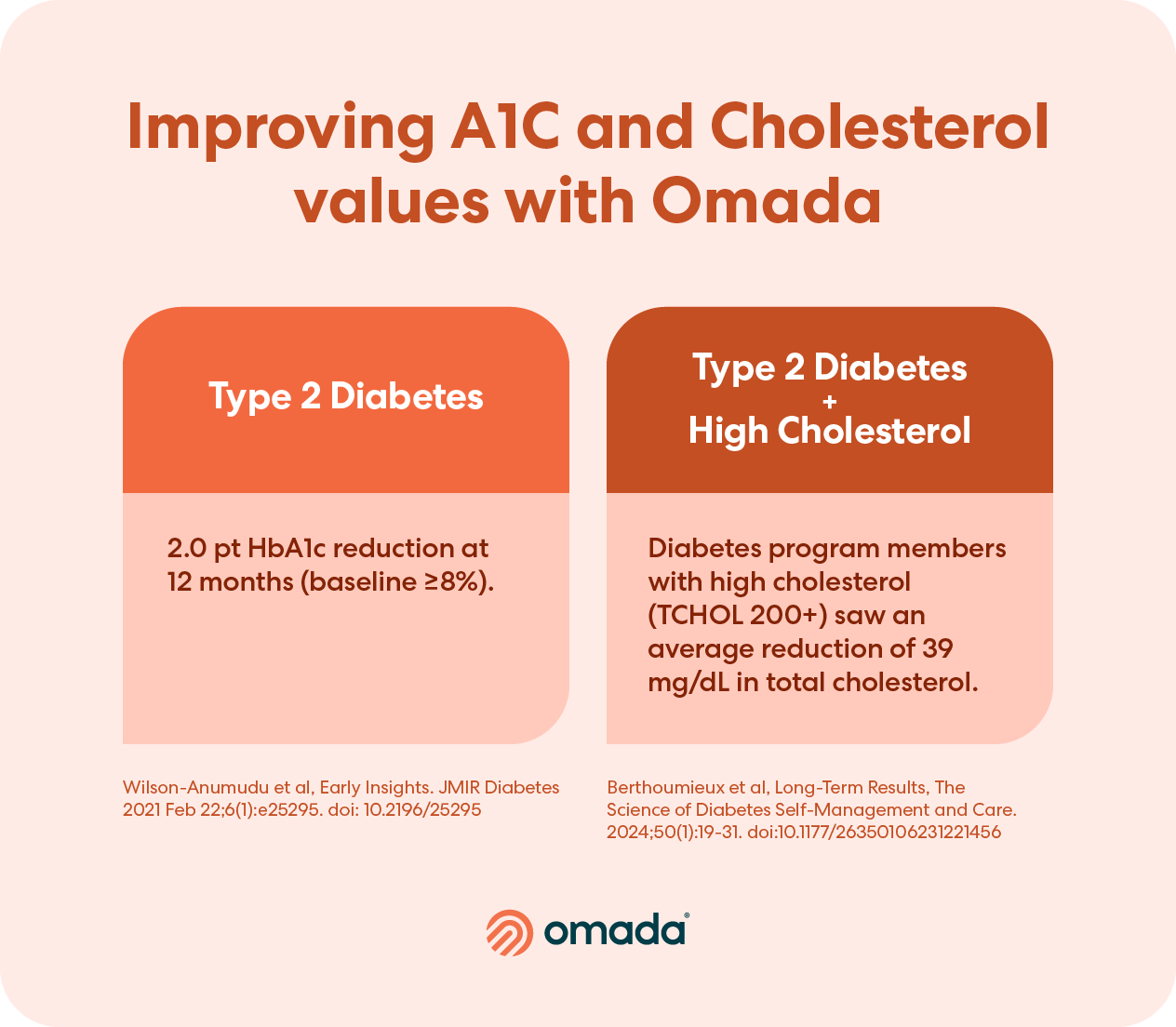
Here at Omada we often say that health happens between doctor’s visits—because it’s true! Daily health behaviors like diet, exercise, stress and sleep have a huge impact on both diabetes and cholesterol outcomes.
That’s why care between doctor’s visits that adapts to the individual is key to realizing better health behaviors that improve blood sugar and cholesterol.
Facilitating a Nutrient-Dense Diet
When it comes to diet, instead of trying to remember the “rules” of a condition-specific eating regimen, we provide tools to help members make diabetes and heart-healthy eating decisions in real time, with a focus on nutrient density rather than calorie counting.

Help Understanding the Numbers
Members may connect their digital devices, such as continuous glucose monitors or blood pressure cuffs, to the Omada app, which gives their care teams access to their health data in real time. This helps Omada care teams provide support and feedback between doctor’s visits. Members can also share lab results such as lipid panels or A1C values for help deciphering what they mean and how they can take manageable steps to maintain or improve their levels.
Medication Assistance
When members share their primary care plan with us, Omada care teams assist with medication adherence, side effects, questions and more.

Diabetes Rarely Acts Alone, and Neither Should We
Understanding the intricate connection between diabetes, cholesterol, and cardiovascular health is crucial for lowering the risk of complications and living a healthier life. But while being equipped with this information is an important step, it’s only the first one.
When I was fresh out of my internship at my first job as a registered dietitian, I’d excitedly tell my patients everything I had just learned about food and health. Who could even hold in all this incredible information? My goal was to impart them with this knowledge so they could use it to manage their cardiometabolic conditions and turn their health around. But as it actually turned out, even after educating folks on an abundance of “fun” (to me) facts about managing their condition, actually applying that education to their daily lives was tough, if not impossible, to do alone.
The challenges of managing multiple conditions can be daunting, from conflicting (or just too much) dietary advice to the complexities of interpreting lab results—on top of everything else we manage day to day as humans.
By providing not only care between doctor’s visits, but care that adapts to the ups and downs of real life, patients can successfully manage their chronic conditions and spend more time enjoying everything else life has to offer.
In my time working in diabetes care, I’ve found that the most successful patients are the ones who seek and accept support. Whether it was support from me, support from their family, support from a virtual provider like Omada, or support from a group, anything helps! But the most successful people choose multiple things at their disposal.
At the end of the day, when it comes to managing multiple conditions, whether for yourself or for your workforce, my two pieces of advice are: know your numbers and never be afraid to ask for help.



