What Everyone Should Know About Menopause and the Musculoskeletal System
This edition covers:
- The impact of menopause on the MSK system and associated risk of cardiometabolic disease
- How declining hormones impact muscles, bones, joints, metabolism and inflammation
- Scientifically backed options for managing symptoms and increasing quality of life
The topic of menopause has gained traction over the last several years, as women’s healthcare startups become more popular among patients. In 2024, the global menopause market was estimated at approximately $17.8 billion, with an expected growth rate of more than 5% by 2030. This is excellent news for women’s healthcare; as the topic of menopause becomes less taboo and more familiar to primary care physicians, women can feel empowered to seek care for their symptoms, and more importantly, care is finally within reach.
Relief from the most well-known symptoms such as hot flashes, night sweats, mood swings and a decreasing libido is the focus of many menopause care solutions, however, the impact of this profound hormonal shift goes much deeper. The Menopause Society defines this natural transition as the period following 12 consecutive months without menstruation, typically presenting in females between ages 45 and 55, with the average onset at 51. It occurs as a result of declining estrogen and progesterone levels, which often results in the symptoms above, but also has a profound effect on the musculoskeletal (MSK) system.
When menopause hits, it can feel like the body is malfunctioning: muscle mass decreases, joints ache, metabolism slows down, appetite ramps up, and the numbers on the scale start climbing. These symptoms essentially create the perfect storm for an increased risk of heart disease, diabetes, and other chronic conditions.
While this isn’t welcome information for anyone entering menopause, understanding the physical impact of this transformation is integral to managing symptoms, mitigating the risk of disease, and improving quality of life both at home and at work. In this article, we’ll examine the physical downsides of menopause, as well as the upside: symptoms can be managed with behavior change and medical interventions.
The Downsides: Declining Hormones Impact Body Systems and Processes
As mentioned above, the two main hormones that change during menopause are estrogen and progesterone.
Estrogen plays a crucial role in maintaining bone density, muscle mass, and overall MSK health.
It keeps bones strong by reducing their natural breakdown, promotes muscle protein production, prevents muscle loss, and may help maintain muscle mass. It is also responsible for suppressing inflammation. Meanwhile, progesterone, which is primarily known as a pregnancy hormone, interacts with estrogen to support bone mineral density and may help regulate muscle mass and strength. When these hormone levels drop during menopause, these safeguards to the bones, muscles and joints go with it, impacting major body systems and processes.
Musculoskeletal Syndrome
When estrogen levels decline in menopause, the effects are seen in the muscles, joints, and bones as a result of increased inflammation from the lack of estrogen. This is known as the musculoskeletal syndrome of menopause, and it is estimated that 70% of all midlife women will experience it. Symptoms include joint pain, loss of lean muscle mass and bone density, increased risk of fractures, and increased tendon and ligament injuries, including frozen shoulder and osteoarthritis. Painful symptoms like these can make everyday activities feel challenging.
Slowed Metabolism
During menopause, dropping estrogen levels can cause the metabolism to slow down and appetite to ramp up, which may lead to weight gain, specifically around the belly. This drop in estrogen along with increased abdominal fat is also associated with a higher risk of heart disease, metabolic syndrome, diabetes, osteoporosis and osteoarthritis, as well as cognitive decline, dementia ,depression, and cancer.
Systemic Inflammation
Inflammation is not only a direct effect of decreased estrogen, but also a sub-symptom of common menopause phenomena such as weight gain, disrupted sleep and lack of physical activity (as a result of MSK pain).
The Upside: The Effects of Menopause Can be Managed
While the physical impact of menopause can sound discouraging, there are strategies to mitigate symptoms and live a healthy, pain-free lifestyle. Most strategies, aside from hormone therapy and anti-obesity medications, are behavioral and can be achieved with the right plan and support.
Strengthening Bones and Muscles
Physical activity is crucial for maintaining overall health, particularly for strengthening bones and muscles. Beneficial exercises include weight-bearing activities like walking and dancing, flexibility exercises such as yoga and stretching, and strength training with weights or resistance bands. Weight-bearing exercises and strength and resistance training can help increase bone density. Wearing a weighted vest while walking might help prevent hip bone density loss and improve bone growth in older adults with obesity. To start using a weighted vest, begin with two to 10 lbs of weight and wear it for 15 to 20 minutes during a short walk.
Strength training exercises that increase muscle mass are particularly important since muscle tissue burns more calories than fat, even at rest. This leads to improved calorie burn, better weight management, and enhanced insulin sensitivity, supporting overall metabolic health.
How much exercise and strength training is needed?
Each week, adults should aim for 150 minutes of moderate-intensity exercise, or 75 minutes of vigorous-intensity activity, or an equivalent combination. Activity can be spread out during the week and broken up into smaller chunks of time. It could be 30 minutes a day, five days a week.
In addition to moderate or vigorous aerobic activity, it is recommended to strength train at least two days a week to increase and maintain muscle mass. For strengthening exercises, a repetition is a single complete movement, and for each exercise, aim to do eight to 12 repetitions as one set; to maximize benefits, complete two or three sets of muscle-strengthening exercises.
Getting the Right Nutrients
During menopause, research highlights the importance of specific nutrients like calcium, vitamin D, magnesium, and vitamin K2 to support bones and muscles. To maintain muscle strength, it is recommended that women in menopause eat 1.0 to 1.2 grams of protein per kilogram of body weight per day.
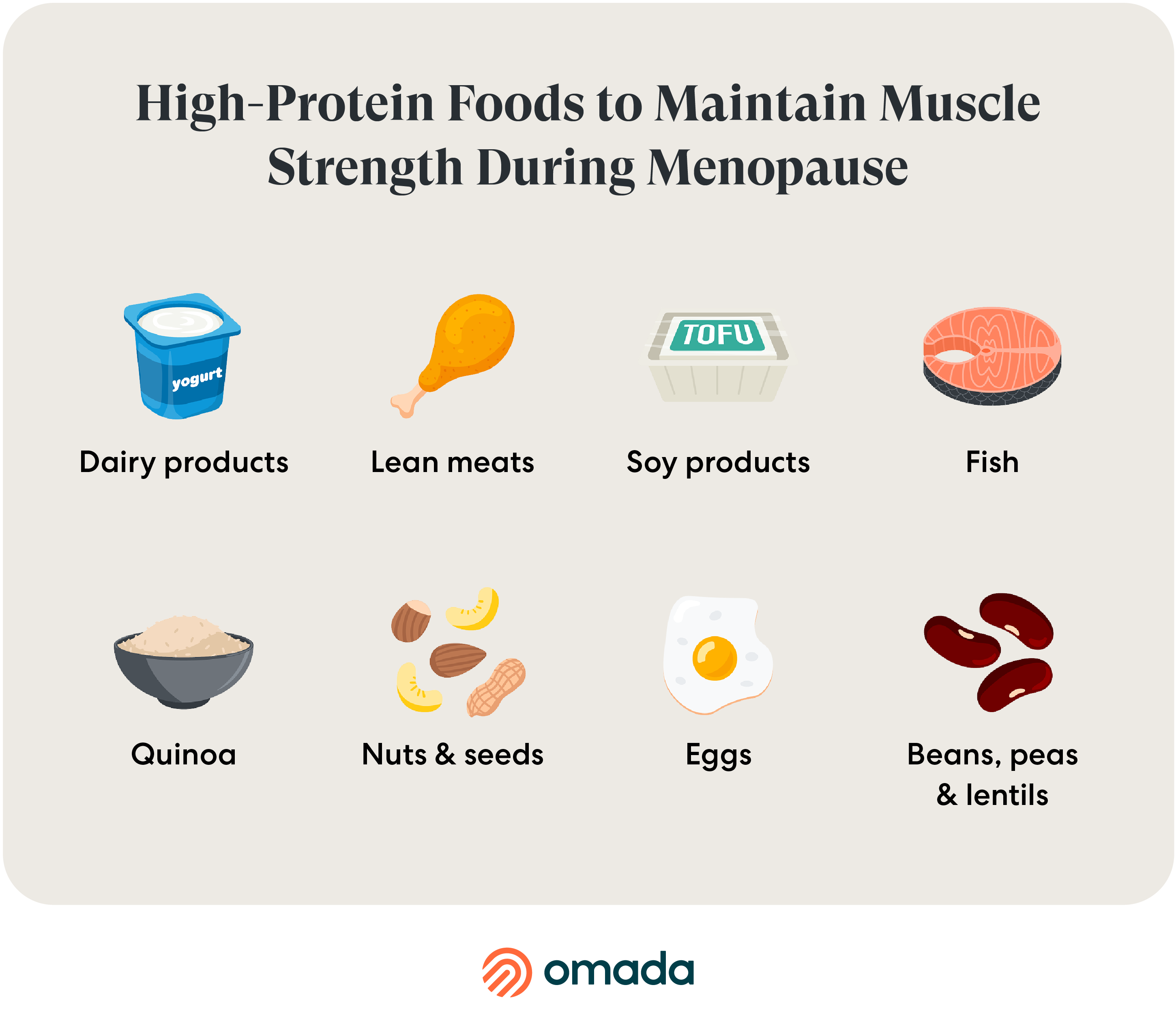
The Mediterranean Diet, which includes foods with anti-inflammatory and antioxidant actions, such as extra-virgin olive oil, vegetables, fruits, legumes, nuts, and whole-grain cereals, has been found to help preserve muscle mass and reduce inflammation.
Avoid smoking and limit alcohol consumption, as both are negatively linked to bone health and an increased risk of cancer.
What about supplements?
Certain supplements may mitigate the MSK effects of menopause, and many over-the-counter products are currently being marketed to menopausal women. Many of these products are not FDA approved, not backed by any scientific research, and certainly cannot “cure” menopause, despite their claims.
To complement a high-protein, anti-inflammatory diet, there are several supplements that are scientifically proven to support bone and muscle health:
Menopause Hormone Therapy and Anti-Obesity Medications
Medical interventions such as menopause hormone therapy (MHT) and anti-obesity medications like GLP-1s can be helpful in managing menopause symptoms. Primary care providers (PCP) should be consulted prior to starting any medical intervention to ensure safety and coordination of care.
Menopause Hormone Therapy (MHT)
Menopause hormone therapy usually replaces estrogen and sometimes progesterone. This intervention can help with many symptoms of menopause. Benefits may include:
- Slowing the loss of estrogen, which can help with joint pain, muscle loss, and bone weakening.
- Preservation of bone mineral density, reducing the risk of fractures that can occur with osteoporosis.
- Help with cartilage issues, and may prevent changes in connective tissue. Think tendons, joints and joint mobility.
- May also help with other symptoms like hot flashes, vaginal dryness, and sleep problems.
Anti-Obesity Medications (GLP-1s)
Anti-obesity medications like GLP-1s are sometimes used when women have tried to modify diet and lifestyle to manage menopause symptoms and are still unable to maintain a healthy weight. These medications may help with reducing fat mass and inflammation, which can decrease joint and muscle pain.
Pairing GLP-1s with clinically proven lifestyle support may be especially effective in managing the musculoskeletal changes of menopause.
The More We Know About Menopause, The Better it Can be Managed
While menopause care has come a long way in recent years, research on this female phenomenon is still limited. The good news is, there is more support than ever by way of specialty clinics and virtual care providers that specialize in menopause, MSK health, weight management and cardiometabolic conditions. As adoption of virtual care providers increases and menopause is researched more specifically by scientists, the healthcare industry will become more knowledgeable about menopause, thus improving care for an estimated 20% of the U.S. workforce.
In the meantime, there are effective strategies to mitigate symptoms and disease risk. Engaging in regular physical activity, adopting a nutritious diet rich in essential vitamins and minerals, prioritizing sleep, and discussing medical interventions with the medical home are all vital components of managing menopause effectively. It is crucial to foster open communication with healthcare providers, seek expert guidance, and build a supportive community, empowering women to navigate menopause with confidence and resilience.